ACO Strategy
3 steps for executing an effective consumer-driven physician strategy
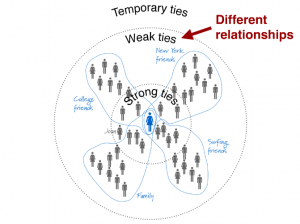
To meet post-pandemic expectations of consumers, healthcare providers need a strategy for consumer-focused care processes, supported by consumer-friendly provider networks and enabling technology.