
There are many good people at the CMS Innovation Center (CMMI). They mean well. They are our friends. But friends need to call out friends when they are out of line.
I received an email this morning from CMS announcing the launch of their new “Value-Based Care Spotlight” website. Right near the top of the main page, CMS asserts their new definition for the term “value-based care.” Although I don’t think there is any conscious conspiracy, I consider it to be another step in a long process of linguistic manipulation that has the effect of misdirecting the public and policymakers away from talking about cost of care and minimizing the risk that someone might accuse CMS of caring too much about money. It represents, in my opinion, a type of denialism of the validity and even the existence of the field of health economics. Let me explain, with as little ranting as I can muster.
You may recall that the original meaning of the acronym “VBC” was value-based contracting. VBC was about financial reimbursement arrangements. The whole point of VBC was to redesign reimbursement contracts between health care payers and providers to better align the providers’ economic incentives with the payers’ objectives and with the associated societal objectives. Payers and the public have an interest in reducing the trend in cost of care growth and to avoid waste due to the unwarranted utilization of low-value health care services and the inefficient delivery of services. The term “value” was intended to mean what it normally means in the field of economics and in common parlance. Value is the difference between the dollar value of the price of something and the dollar-value of the net benefits that accrue from the thing. Something is described as being a “good value” when the benefits are high in relation to the price. It is not a technical term. It is a term that has a common, plain meaning. In our field, “health care value” has been a topic that is all about addressing concerns about long term increases in healthcare costs that have not been justified by sufficient improvement in health care outcomes.
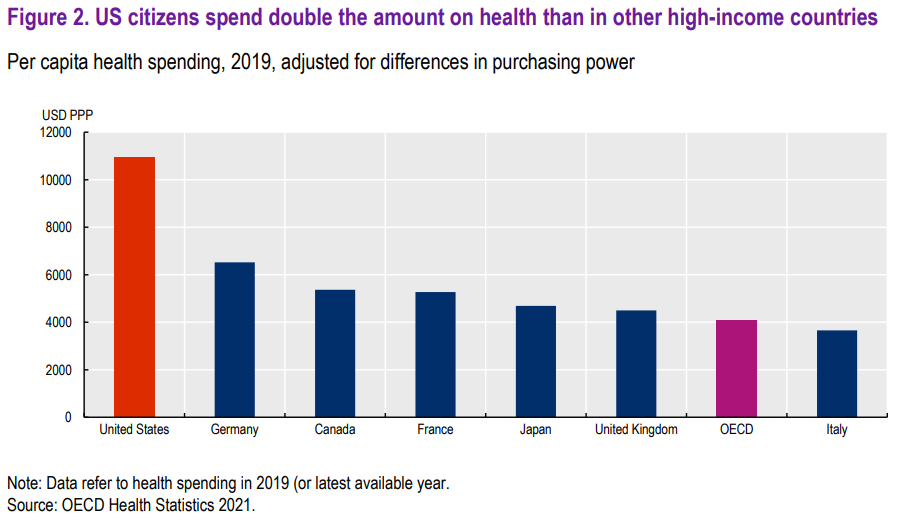
Compared to all the other OECD countries, our total cost of care per capita has long been twice as high and our outcomes are generally no better. So, a concern for health care value is clearly justified.
But, right from the beginning, there were many health care leaders, including leaders at CMS, that felt uncomfortable about the focus on health care costs implied by the term VBC. I assume that one source of this discomfort was the longstanding American denialism of the principles of health economics, a topic of many posts in this blog, particularly this blog post from 2011. This health economics denialism has been the source of previous mischief, such as federal policies prohibiting the use of “quality-adjusted life year” (QALY) metrics by government agencies, misinformation about “death panels” in health care reform legislation, and the use of the word “rationing” in a way that implies it is something done by evil villains twisting their mustaches, rather than virtuous attempts to allocate finite resources in a rational way to maximize population benefits. Even healthcare leaders that care about total cost of care are eager to avoid being accused by others of putting dollars above patients. I assume that another potential source of the discomfort with a focus on health care costs has been the idea that such a focus was in competition with what many felt were higher and more urgent priorities, such as efforts to expand access to care, reduce disparities in care, and address social determinants of health.
But, whatever the justification, many health care leaders and many CMS leaders have been working for a long time (unconsciously perhaps) to take the original meaning of VBC and drag it to the deep end of the pool to drown it. First, they got rid of the dirty word “contract” and the implied focus on money and replaced it with “care.” Now, they have redefined value-based care to completely eliminate any reference to cost, efficiency, waste, economics and finances. In the new CMS definition, value-based care is defined to mean “health care that is designed to focus on quality of care, provider performance and the patient experience.” But they still were worried that the word “value” retains some connotation of economic value. So CMS has now clarified that they mean something different, stating “the ‘value’ in value-based care refers to what an individual values most.” Everything is about the individual patient experience and the individual patient preferences. Nothing about payer, population or society. Nothing about cost. VBC is now just a synonym for “quality” or perhaps “goodness and light.” It has been drained of meaning.
I find this terminologic warfare within our field to be a dishonest and manipulative process, even if well-intentioned. We should be better than that. My preference is to first talk about health care operations and then describe the financial arrangements needed to enable them.
When describing health care operations, I like to use the term “population health.” It connotes a sense of responsibility that goes beyond just reacting to the problems of individual patients that present themselves to a clinician. It implies that we should also take responsibility for a population. Taking responsibility for a population implies the need to be proactive. It also implies a duty to consider the outcomes experienced by the population collectively. In the context of private health insurance and government payers, the cost of care is experienced collectively by the population (as employees, business owners and taxpayers), not just in the form of patients’ out-of-pocket expenses. Therefore, population health implies a duty to be good stewards of limited economic resources. Stewardship is a virtue, not a vice (reference: Matthew 25.14-30).
When referring to health care operations, I also like the term “clinical process improvement” (when talking to clinicians) or “care process improvement” (when talking to non-clinicians). These terms emphasize the fact that outcomes are achieved not just by individual providers’ heroic “performance” but through processes — including both care planning (decision-making) and care delivery processes. Processes involve teamwork and organizations. Process improvement implies that our responsibilities go beyond just executing care for individuals to include proactive and systematic efforts to improve those processes over time.
Only after talking about health care operations, using terms such as those proposed above, should we then talk about the enabling financial arrangements. I like to use the term VBC in its original meaning: “value-based contracts.” I prefer that the term VBC merely refers to the structural/contractual/financial mechanisms to enable care providers to capture a reasonable share of the resulting economic value created as needed to make the operations sustainable and to motivate and provide returns on the investments required to improve those operations. Contracts are about money. That’s not evil. We can and must be honest and clear. So, CMMI friends, please desist with the VBC doublespeak.
















2 thoughts on “CMS Innovation Center engages in linguistic manipulation and health economics denialism in new definition of “VBC””
Dr. Ward, thank you for raising this important issue. You are absolutely correct in your assessment of how CMS has consciously twisted the VBC moniker to suit its political messaging to its stakeholders. That being said, the foundation of VBC is really the re-distribution of risk from the payer to the provider, which is a euphemism for capitation, a dirty word amongst physicians and other healthcare providers. Since it’s a long arduous journey for providers to become weaned from the fee for service world, as long as we’re moving towards the VBC direction, even if using different definitions of “C,” it will be a win for American healthcare. Keep leading the good fight, Dr. Ward!
Dr. Pan, great to hear from you! I agree that many physicians currently see “capitation” as a dirty word. I think that’s because they’ve been harmed in the past when they have felt pressured to enter into provider-payer contracts where they took on more risk than they could handle. But, as you know well from your work with California medical groups that successfully handled substantial risk, physician groups that make investments in population health and sophisticated analytics are in a better position to manage risk in an informed and ethical way than any health insurance company or government agency. As you noted, we just need to keep up the good fight.