
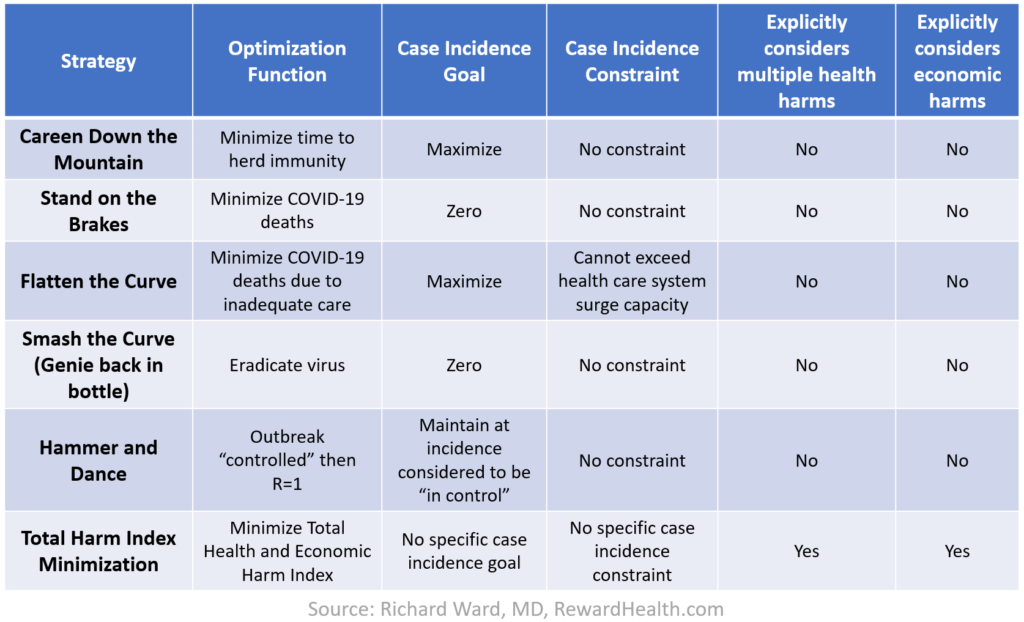
In my last post, I described three helpful analogies — Forest Fire, Genie in the Bottle, and Trucker in the Mountains — that make it easier for leaders to wrap their heads around different COVID-19 pandemic response strategies. In this post, I will use those analogies to explain six COVID strategies:
- Careen Down the Mountain
- Stand on the Brakes
- Flatten the Curve
- Crush the Curve
- Hammer and Dance
- Harm Index Minimization
Then, I will explain why one of these strategies — Harm Index Minimization — is the best, and how we are working to provide analytic innovations to enable it.
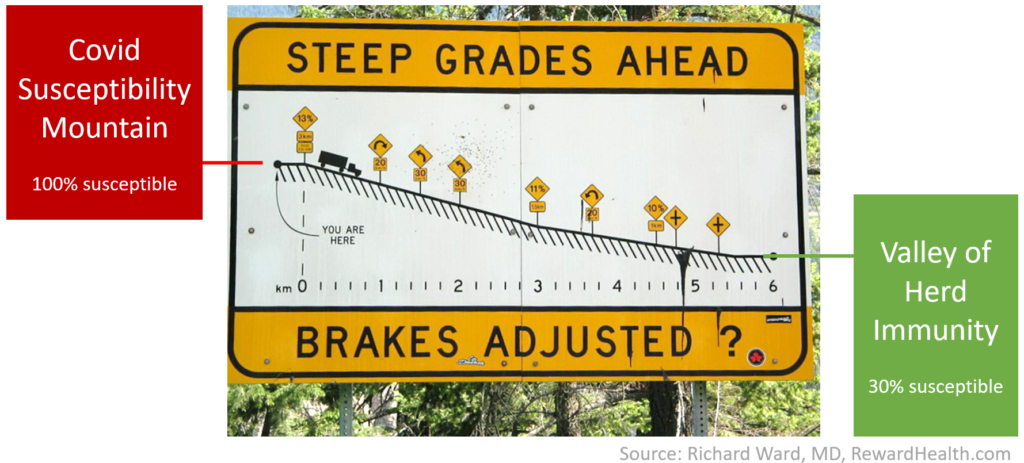
In the “Trucker on the Mountain” analogy, we imagine ourselves as drivers of an 18-wheeler truck near the top of Covid Susceptibility Mountain at the beginning of the pandemic. At that point, nobody had been infected by COVID-19 and there was no vaccine, so nobody was immune and everybody was susceptible to infection. The truck has to make its way down the mountain on a steep, twisty road. There are dangerous cliffs and no guardrails. We need to descend the mountain to reach the Valley of Herd Immunity, where most people are immune from COVID-19 because they were infected and recovered from it already or they have been vaccinated. In the valley, the trucker is safe because the virus has trouble finding enough susceptible people to keep spreading and the pandemic stops or slows down to a manageable speed.
Let’s use this analogy to understand the six pandemic response strategies.
Careen Down the Mountain Strategy
This could also be called the Sweden Strategy because it was widely understood to be the unofficial strategy underlying the permissive COVID-19 pandemic response policy developed by Anders Tegnell, the Swedish state epidemiologist, particularly during the earlier stages of the pandemic.

The strategy calls for the truck driver to drive full speed down the mountain road, delivering his cargo on-time and getting to the Valley of Herd Immunity as quickly as possible. The implicit goal of the strategy is to minimize the economic harms that would be caused by slowing down the economy. As suggested by the word “careening,” the downside is the risk of death from driving off a cliff — letting the exponential spread of the virus overwhelm the health care system, leading to infected patients being treated in tents, patients dying for lack of access to limited-capacity health care resources such as ICU beds, ventilators or drugs, and hospital staff dying for lack of personal protective equipment. An out-of-control outbreak can even overwhelm the capacity of mortuary resources, evidenced by bodies stored in refrigerated trucks (as occurred in New York) or on the ice in a skating arena (as occurred in Spain).
This Careen Down the Mountain strategy is only an implicit strategy. In the US, this approach has reportedly been advocated by Scott Atlas, MD, a fellow at the Hoover Institute who joined the White House recently as a pandemic advisor, but the White House denied pursuing such a policy. Even in Sweden, it was not explicitly acknowledged, presumably because the sacredness of human life is an unassailable principle in all but the most depraved settings. Consequently, the public face of such a strategy has taken the form of denial of the severity of the pandemic – such as when COVID-19 is compared to the flu or when leaders predict the imminent spontaneous end of the pandemic.
Stand on the Brakes Strategy

This is opposite of the Careen Down the Mountain strategy. The goal is to minimize COVID-19 deaths by bringing the truck to a complete stop as quickly as possible near the top of Covid Susceptibility Mountain — by pursuing the most aggressive virus containment and mitigation policies and interventions that can be mustered.
The most potent of such policies is an enforced “stay-at-home” or “lock-down” order. Other policies include shutting down international and interstate travel, closing factories, retail locations, schools, restaurants, and other places and events where virus transmission can occur, strictly enforcing social distancing and mask wearing, and doing intensive surface cleaning of streets and public facilities.

These policies remain in place until a vaccine has been developed and administered to a substantial portion of the population — like a giant helicopter rescuing the truck and safely delivering it to the Valley of Herd Immunity.
The obvious disadvantages of the Stand on the Brakes strategy are the short and long term economic harms associated with the shut downs, along with the health harms that are not directly attributable to COVID-19. Two recent studies by Weinberger and Woolf have shown excess non-COVID-19 attributable mortality of 22% and 35%, respectively, during March-May, 2020, compared to prior years. Some of these excess deaths are presumably due to under-reporting of COVID-19 deaths. But others of these excess deaths are likely due to under-treatment of other diseases due to lack of access to health care when clinics and procedure rooms are shut down or people could not afford care. Still other excess deaths are consequences of the economic harms, as evidenced by spiking rates of opioid overdoses and homicides that have been observed in some cities during the COVID-19 pandemic.
To maintain political will and reduce short term economic suffering due to the Stand on the Brakes strategy, deficit spending can support unemployment benefits and other social and economic supports. But, due to the long timeline to develop and broadly administer a vaccine, a rigorous, ongoing application of the Stand on the Brakes strategy is unlikely to be a realistic strategy for COVID-19.
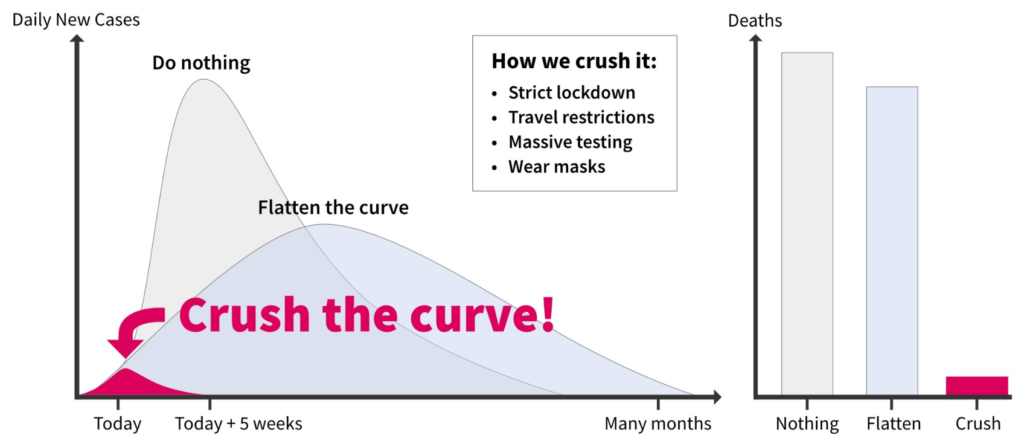
Flatten the Curve Strategy
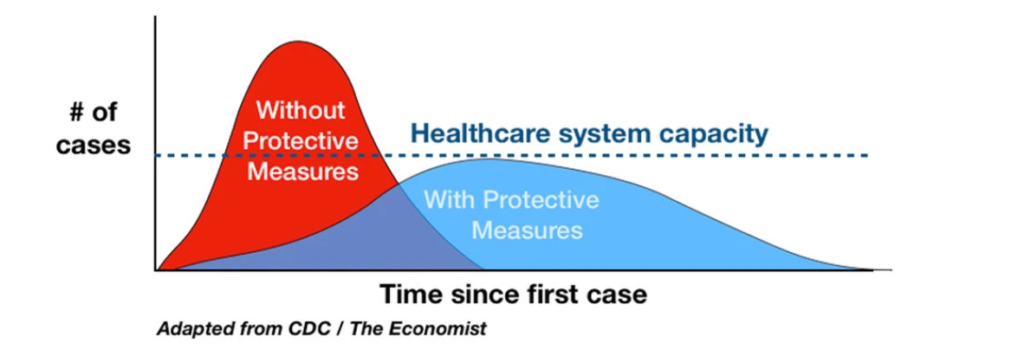
The traditional approach to dealing with outbreaks with substantial community transmission, as taught in schools of public health and endorsed in the playbooks of the CDC and the WHO, is the “Flatten the Curve” strategy. This strategy is illustrated in the diagram above, which depicts the pandemic as a single-hump curve that could be flattened — shifting the area under the curve (total cases) toward the right to keep the peak from exceeding the number of cases that could be handled by the health care system, even after adding surge capacity. Similar diagrams are found in epidemiology text books and were widely disseminated and discussed during the early stages of the pandemic.
Using our analogy, in this strategy, the truck driver proceeds carefully down the mountain road, tapping the brakes as needed to maintain a safe speed. The strategy implicitly accepts that it would be too economically harmful to just Stand on the Brakes. It also implicitly accepts the inevitability of continued spread of the virus through the population: the truck is still going down the mountain. In the Flatten the Curve strategy, the focus is on trying to keep the truck from careening out of control, overwhelming the capacity of the health care system — particularly hospital beds, ICU beds, respirators, personal protective equipment and other limited resources that are required to treat infected patients and reduce risk to health care providers.
As with the Stand on the Brakes strategy, the stated objective of the Flatten the Curve strategy is to reduce COVID deaths. But the key difference is that Stand on the Brakes is trying to avoid COVID deaths by preventing all COVID infections, while Flatten the Curve is focused on avoiding the subset of COVID deaths attributable to lack of good health care due to an overwhelmed health system.
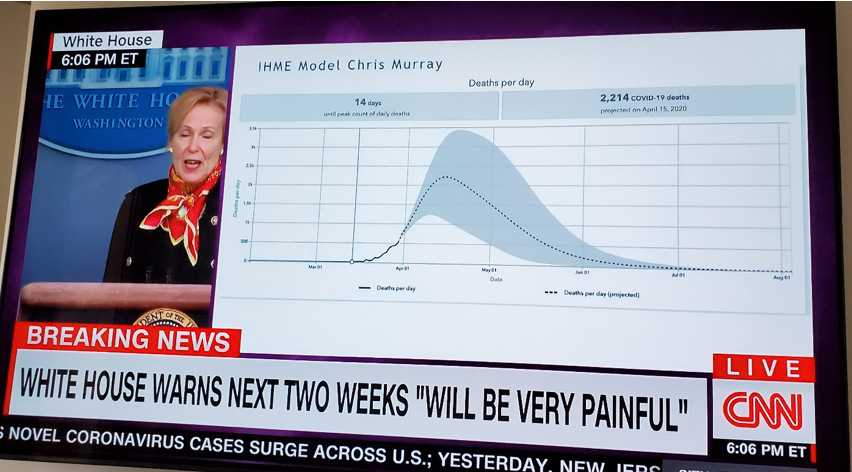
To guide pandemic response planning, computer-based models are used. The COVID-19 pandemic model that has been most prominently used by the White House and in cable news reporting — developed by Chris Murray and colleagues at the University of Washington — used a model structure that assumed a single curve, resembling the traditional one-hump Flatten the Curve diagram.
Other models have been developed using different modeling methods that were not structured to assume a single hump. One prominent example is the model developed by Neil Ferguson and colleagues at Imperial College, which is an agent-based model that has been used to guide some national policy-making in both the U.K. and the U.S.
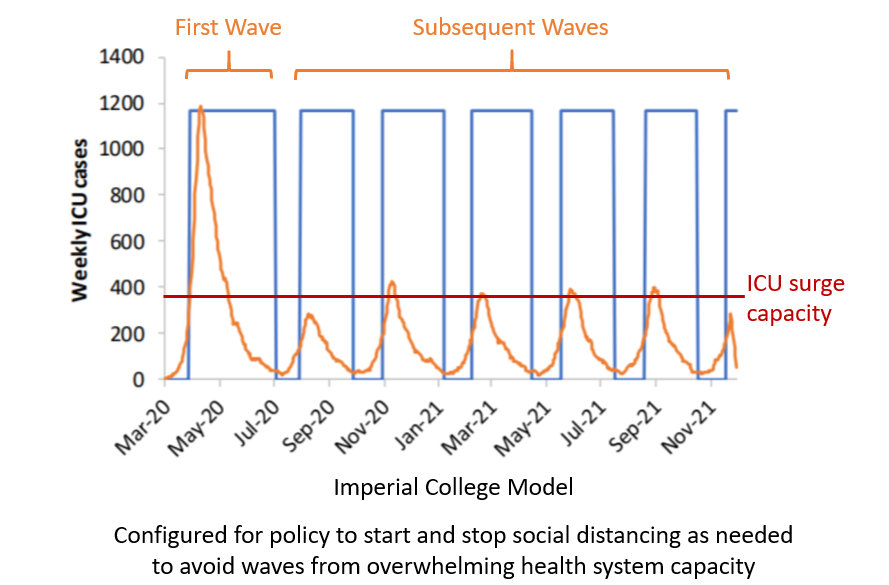
As shown in the diagram above, the Imperial College Model was configured for a scenario in which, after an initial out-of-control wave that exceeded ICU surge capacity, a policy was put in place to shut down parts of the economy and take other mitigation measures during periods of time shown as blue boxes — analogous to tapping the brakes on the truck as needed to keep the speed from exceeding the surge capacity of ICU beds. The brakes are then released once the speed gets back under control to avoid overheating, causing the speed to begin to pick up again. This cycle of braking and picking up speed is repeated through the end of 2021, when the truck reaches the Valley of Herd Immunity. Note that based on the Imperial College Model (as of April, 2020), the economically harmful mitigation measures need to be in place two thirds of the time, with a month of reprieve every few months — predicting a dreary, exhausting two years.
Crush the Curve Strategy – AKA Genie Back in the Bottle Strategy

Recognizing the economic in-feasibility of the Stand on the Brakes strategy and the dreariness of the Flatten the Curve strategy, some have fantasized about a Crush the Curve strategy, where the initial lock-down is enforced so rigorously and other mitigation steps are so severe and effective that we can get the number of cases down to a level where containment and eradication efforts are possible, after which it will be safe to re-open even without a vaccine.
As shown in the diagram above, tweeted back in April, 2020, the Crush the Curve strategy is a no-brainer when you are at the beginning of an outbreak, in what epidemiologists and public health officials call the containment phase. If there is a report of an outbreak of a bad disease in a rural village somewhere, epidemiologists heroically helicopter into the area. If they can establish a perimeter, identify all the cases, do careful contact tracing and enforce strict quarantines, there is an opportunity to nip it in the bud while the outbreak is still on the flat part of the exponential growth curve. If the detection of the outbreak is delayed or the epidemiologists fail to respond quickly enough, they could find that the outbreak has already started to spread. At that point, containment is much harder, but it may still be possible. With a strong enough lock-down, the outbreak may be slowed to the point that cases go back down to a level were containment activities can be successful. The genie can be stuffed back into the bottle.
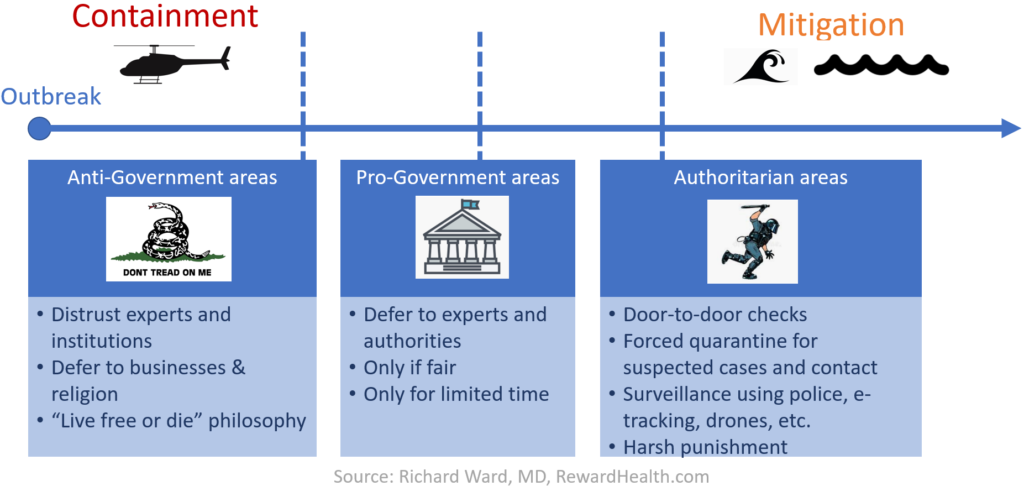
Epidemiologists and public health officials recognize that there is some boundary separating the containment phase (when the outbreak can be contained and hopefully eradicated) from the mitigation phase (when eradication is futile and the goal is just to reduce harms). Depending on the setting, that boundary can shift. In authoritarian areas, more extreme containment measures are feasible. In areas where people have a strong distrust for experts and institutions and the people profess a “live free or die” philosophy, containment becomes unattainable at an earlier stage in an outbreak.
In the case of the COVID-19 pandemic, we clearly missed the opportunity to nip it in the bud, both in Wuhan, China and in the period during which the first few cases were discovered in the U.S. and Canada. Community spread is obviously widespread, with over fifty thousand new known cases per day, and many more unknown cases. So, in the current context, is the Crush the Curve strategy really relevant?
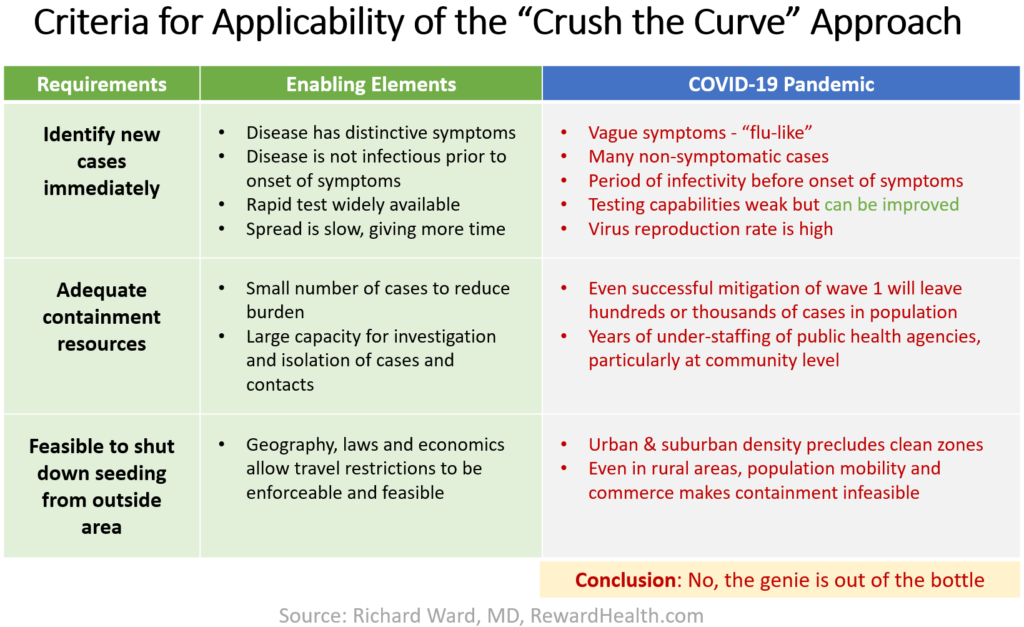
As shown in the table above, the COVID-19 pandemic has characteristics that are incompatible with success of the Crush the Curve strategy. At this stage of the pandemic, the Genie is Out of the Bottle and we are very unlikely to convince the Genie to go back in.
The Hammer and Dance Strategy

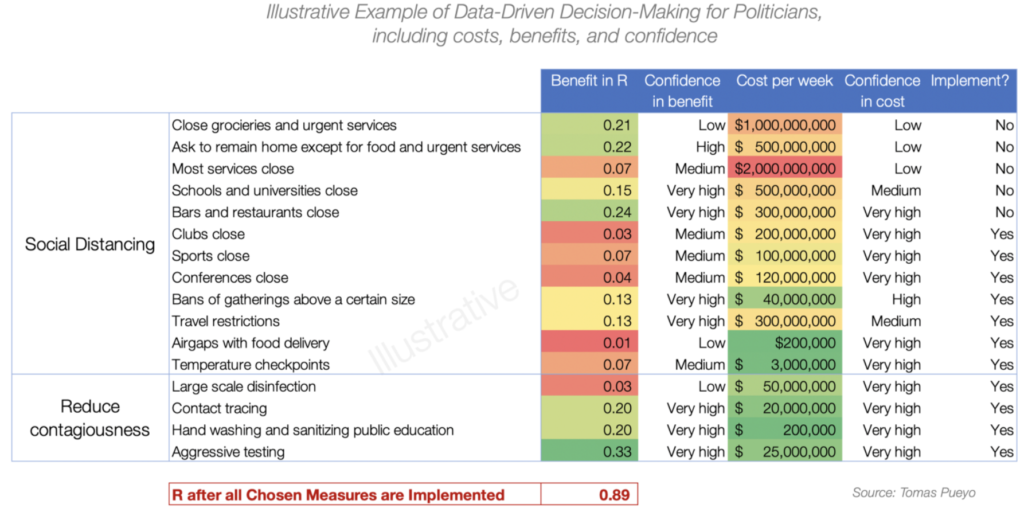
This strategy, elegantly and thoroughly explained by analyst and blogger Tomas Pueyo in a widely-discussed post back in March, 2020, is a more realistic variation on the Crush the Curve approach, emphasizing a period of lock-down and other severe mitigation policies to dramatically decrease the rate of new cases. In other words, crush = hammer = slamming on the brakes. The difference is that while Crush the Curve has the objective of reducing the virus to the point of containment (Genie back in bottle), the Hammer and Dance approach recognizes that containment and eradication are infeasible. We can only hope to get the virus down to some level where we no longer consider it to be “out of control” and then work to maintain control until a vaccine can be developed and broadly administered. In this strategy, that process of maintaining control is called the “Dance of R” — a process of implementing policies and programs designed to keep effective “R” value, the rate of spread of the virus, close to 1, which corresponds to holding the new case rate constant. Relating back to the Trucker in the Mountains analysis, the strategy is to acknowledge that the truck is going a dangerously high speed, slam on the brakes to get back to some slow, controlled speed “X”, and then operate the gas pedal and brakes to maintain a constant speed X.
Hammer and Dance strategies were proposed early in the epidemic, and adopted explicitly in some countries that have achieved early success in their pandemic response, including Denmark and Norway. But, in the U.S., the initial hammering, crushing and brake tapping was too timid and too short, and the truck has continued to careen at a troubling speed, leading to renewed proposals consistent with Hammer and Dance. In a New York Times Op Ed on August 7, 2020, Michael Osterholm (University of Minnesota) and Neel Kashkari (Federal Reserve Bank of Minneapolis) proposed a “lock-down” of up to six weeks with a specific goal to get the new case rate for any particular area down to one case per day per 100,000 population, asserting “that’s the point at which we will be able to limit the increase in new cases through aggressive public health measures, just as other countries have done.” The proposal was amplified the following day by the Editorial Board of the New York Times who asserted that a strict lock-down for 6 weeks would “get the virus under control.”
The Dance phase involves a mixture of policies for social distancing and reduction of contagiousness that increase or decrease the rate of spread “R.” Therefore, Pueyo’s “Dance of R” requires analytics to support “data-driven decision-making” as Pueyo explains using the following illustrative example (not real numbers).
Everything is right about this strategy except for one thing: it offers no explicit guidance about speed X. Pueyo says:
“Once the Hammer is in place and the outbreak is controlled, the second phase begins: the Dance.”
But what is the definition of “controlled?” How do leaders decide what speed the trucker should maintain during his long dance down Covid Susceptibility Mountain? (My high school Literature and Composition teacher, Mrs. Fryzel, would be aghast at the mixed metaphor.)
Harm Index Minimization Strategy
From my perspective, the best strategy is to approach the pandemic response as an optimization problem. In my experience, most hard problems are optimization problems, where there are multiple conflicting objectives and the extremes are undesirable.
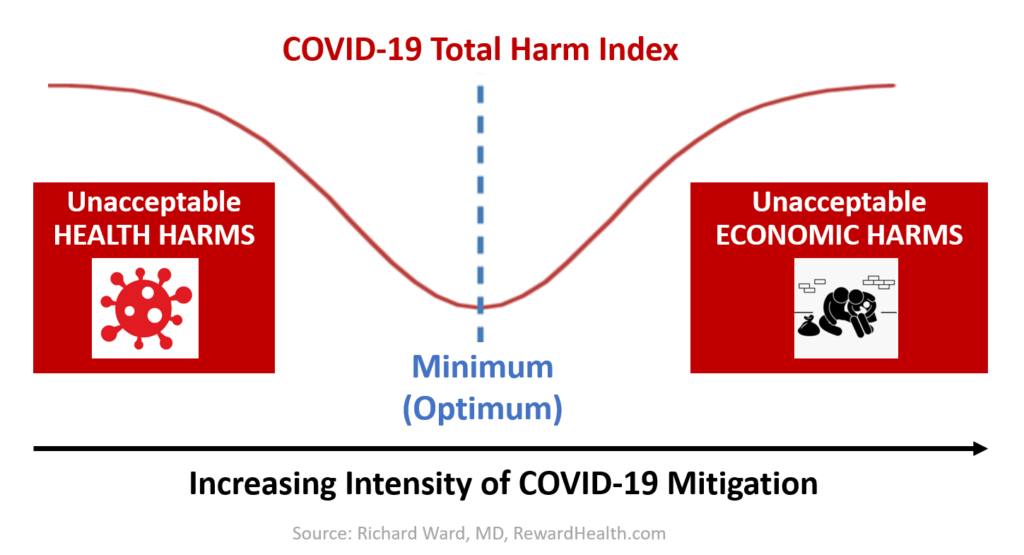
In the case of COVID-19, if we Careen Down the Mountain, we can expect to suffer an unacceptable risk of death and other health harms. If we stubbornly Stand on the Brakes, we face an unacceptable level of economic harm. Therefore, as with the Flatten the Curve and Hammer and Dance strategies, we need to tap the brakes periodically and carefully make our way down the mountain to reach the Valley of Herd Immunity.
However, we need to be clear and thoughtful about our optimization function — the metric that best reflects the thing we are trying to maximize (if it is a good thing) or minimize (if it is a bad thing). In the case of the Flatten the Curve approach, if you really think about it, the optimization function is to maximize the allowed rate of new infections within the constraint that the health care system capacity cannot be exceeded. That optimization function makes sense from the perspective of health care leaders, who naturally want to avoid feeling bad about people dying because they could not offer the care that their infected patients needed. In the Hammer and Dance strategy, the optimization function is to maintain constant “R” after reaching a case rate of “in control.” That makes sense from the perspective of epidemiologists and public health leaders, who naturally want to win their battle against an “out of control” epidemic.
But, these optimization functions do not make sense from a societal perspective — which is the perspective that should be taken by government leaders. In my opinion, it is also the perspective that should be taken by health care delivery system leaders and public health officials, despite the fact that many such leaders and officials are unaccustomed to accepting responsibilities that extend beyond the health domain.
In my opinion, the true objective — the optimization function — should be to minimize the total health and economic harms from a societal perspective. This is a utilitarian strategy, as originally defined by Jeremy Bentham. I would argue that it is also a humanitarian strategy.
As we learned in high school philosophy class, Bentham is not the only ethical philosopher. Accordingly, as we evaluate total harm minimizing strategies, we can also constrain the optimal solution based on other societal values and ethical principles such as social justice, constitutionality, simplicity and standards of evidence. Nevertheless, I think the starting point should be utilitarian analytics, and the other principles should be secondary constraints applied to candidate utilitarian solutions.
To pursue the Total Harm Minimization strategy, we obviously need to define “total harms.” To be able to total the harms, they must be expressed in a quantitative way — as harm metrics. Therefore, as a prerequisite to pursing this strategy, each community must clarify the metrics that are available or feasible to develop and that represent the important health and economic harms that are likely to be different under different COVID-19 policy and mitigation program scenarios.
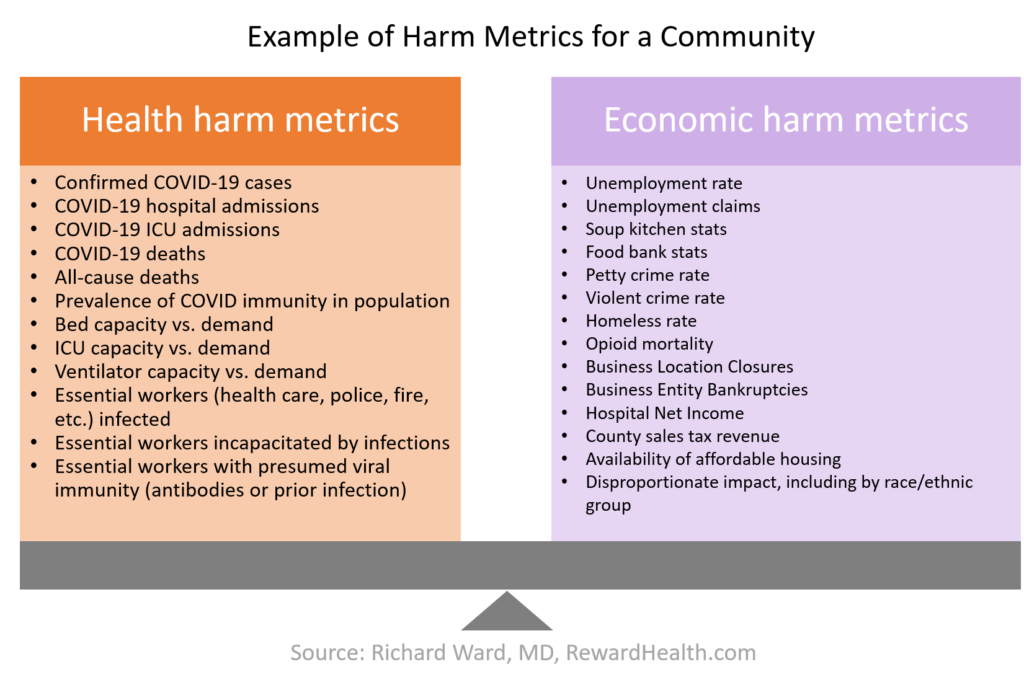
Considering economic harms is not a matter of trading lives for dollars. Deaths from COVID-19 and deaths from opioid overdoses or murders caused by pandemic-related economic strife are all real deaths. The experience of a frightening hospitalization for COVID-19 and the experience of episodes of hunger or housing insecurity caused by COVID-19 shut-downs are also real harms that are experienced by real people. Our objective is to minimize all those harms.
Obviously that does not mean that all outcomes – deaths, sniffles, cases of unemployment — are counted equally. There is no way around having to consider relative values of different types of harms. Therefore, each community must clarify the relative importance of the different types of health and economic harms for which they have identified relevant metrics. They need to agree on some reasonable point system or weights that reflects the values and priorities of the community.
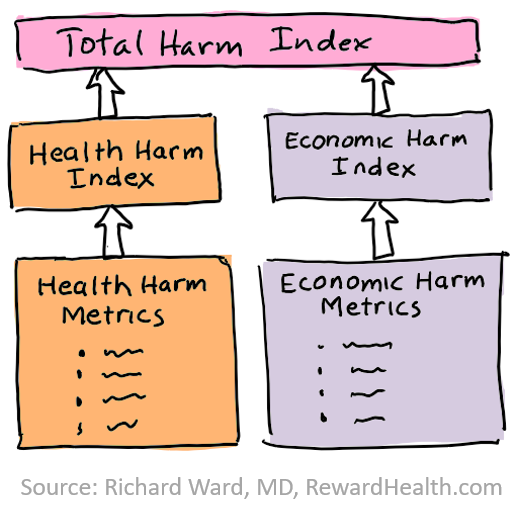
Based on these points or weights, the health harm metrics can be summarized into an overall health harms index, and the economic harm metrics can be summarized into an economic harm index. Finally, both indexes can be summarized into a COVID-19 Total Harm Index. All the individual metrics are important to tell parts of the story. But the COVID-19 Total Harm Index provides the simplest possible quantitative way to summarize the multiple important pandemic outcomes. This is a unitless metric, not measured in dollars or lives. People are familiar with dealing with such unitless metrics, such as with credit scores and stock market indices.
Summarizing the Six Strategies
A new class of models is needed
Most of the prominent pandemic models that have been used by leaders during the COVID-19 pandemic, including famous models from the University of Washington, Columbia University and Imperial College, calculate cases, deaths and health resource demand. But to enable Total Harm Index Minimization, pandemic models are needed that calculate the harm metrics and indices. Such new models should be used by county commissioners, governors, leaders of public health agencies and health care delivery systems, and pandemic task force members to compare alternative proposals for COVID-19 mitigation policies and programs in a way that is holistic but still quantitative — again reflecting the values and priorities of the community.
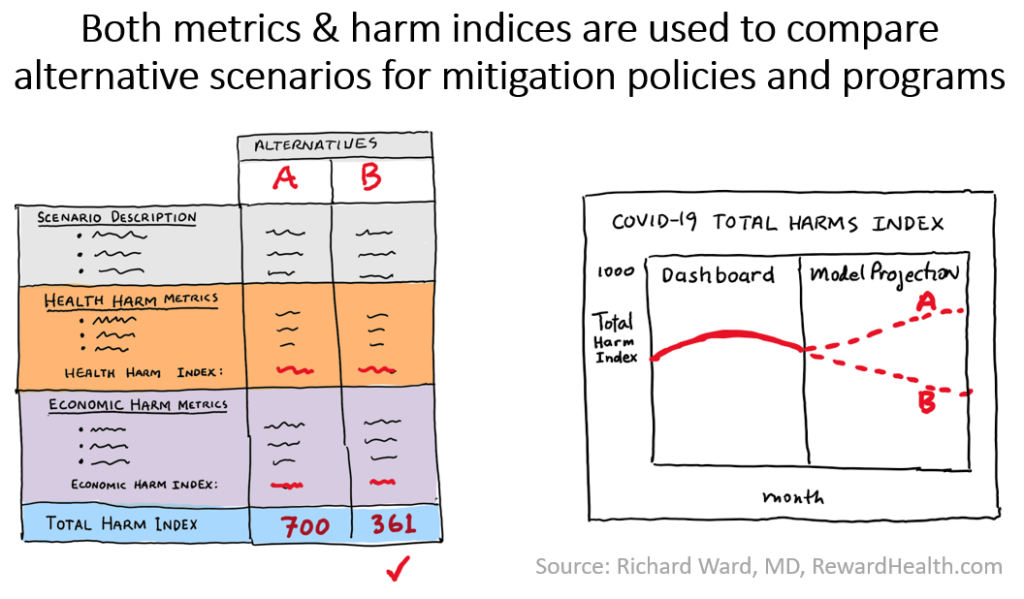
Such new Total Harm Index models can also be used to track progress of the pandemic response in a community and to make predictions about future progress, allowing the public to understand the trade-offs of health harms and economic harms and to hold leaders accountable — for making or not making choices that are true to community values and for successful execution according to those choices.
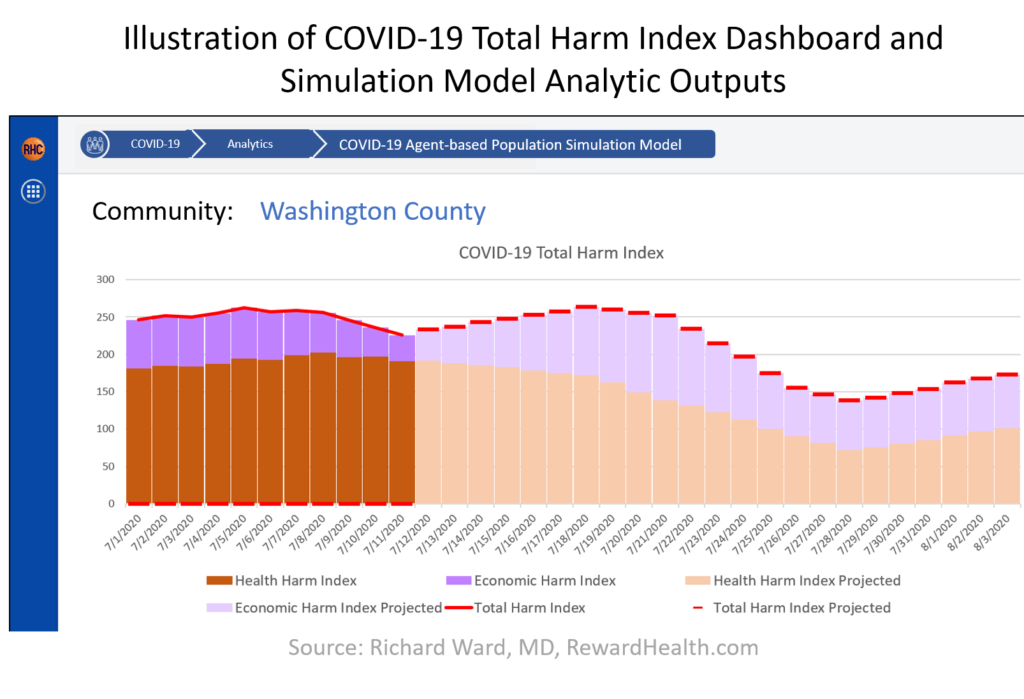
These dashboards and models are the analytic prerequisites for pursuing the optimal COVID-19 pandemic response approach: the Harm Index Minimization Strategy.
That’s why we are focusing on these analytic innovations at Reward Health. We are eager to hear your perspective. And we are eager to recruit collaborators to make this Harm Index Minimization Strategy a reality.

















6 thoughts on “Introducing the Harm Index Minimization Strategy for COVID-19 pandemic response: Better than Flatten the Curve, Crush the Curve and Hammer and Dance strategies”
Thank you for a thoughtful, entertaining, creative and helpful analysis.
My question relates to quantifying and prioritizing at a community level when the topic is so complex, filled with qualitatively different variables. Often our opinions on how much value should be attached to prosperity vs. safety differs from our actions. When evaluating Quality Adjusted Life Years (QALY) saved, the questions are put into operational terms, such as, “if you were paralyzed and a procedure with 50 percent mortality was available with 100 percent certainty of curing the paralysis, would you choose the procedure?” This supports a quantitative analysis that includes personal values and choices. Those who proclaim, “Live free or die!” may feel this way as long as the risk of their own death is very low, but it places little value on the risks born by others infected by persons with this perspective. So, how would we conduct a thoughtful process leading to a rationale decision reflecting true values held by the community?
I had a few observations after reading through this well thought out approach:
1) The “Hammer and Dance” method seems like it is an example of the Harm Minimization approach playing out, in that there is an implicit balancing of interests within both the early pandemic ‘Hammer’ phase and the later pandemic ‘Dance’ phase. During the early pandemic phase, there may be natural changes in behavior patterns which may be either rational or irrational (changing consumer behaviors such as increased purchasing of groceries, less spending on clothing, fewer real estate viewings, and cancelled medical appointments for health systems treating cases). Policies implemented during this phase, when we know the least about the pathogen, may be economically or socially constructive in dealing with irrational behaviors while also potentially being economically or socially destructive in accordance with encouraging rational behaviors. With increased knowledge about the pathogen, policy choices can be re-evaluated during the ‘Dance’ phase for their health, social and economic impacts.
2) Is the goal to measure the adverse social and economic consequences with the same cadence as the health impact? If so, do we have the data sources that are amenable to the daily measurement as is the case with the health impact? Or instead, should we pre-define policy choices such as the closing of schools, closing of indoor dining, or cancellation of large outdoor events and evaluate the impact of each of these decisions prior to the next pathogen? If we expect these policy choices to have fairly similar economic and social impacts regardless of the pathogen, then it seems feasible that these impacts could be determined ahead of time without the need to model them simultaneously alongside the health impacts. A challenge here is the ability to differentiate the effect of the pathogen (letting natural behavioral pattern changes play out) and the effect of the policy decision being made.
3) A potential alternative approach based on a predetermined set of policy effects is to set up a gated response that coincides with something like hurricane tracking. As the storm forms out in the ocean (case counts are low but the reproductive number is over 1), you simply watch and see what happens. Once the storm establishes itself and moves closer to land (case counts are still manageable but increasing and the reproductive number is still too high), you begin initial preparations with policies that have significant health benefit with lesser economic and social consequences. If the storm continues to intensify, so to do the policy choices until either the storm goes off course or until it hits and your preparations allowed you to blunt the worst of it.
4) Measure selection would require a level of community input, but may be important to look at larger constructs identified. Opioid deaths and suicides could be evaluated separately or combined under deaths of despair due to the higher levels of unemployment associated with the policy decisions. However, there is also a paradoxical relationship in that during times of recession, overall population mortality typically declines because there are fewer deaths from other sources such as motor vehicle accidents. It’s unclear if this relationship would hold for a pandemic-induced recession. So should we examine deaths of despair or all causes of mortality in the list of harms? QALYs may be one way to combine all of this together for better comparison. There have also been methods for assessing and combining harms that are used in hospital patient safety measures that could be useful here. Also, how much emphasis should be put on short-term outcomes (hospitalization) and long-term outcomes (lifelong disability or disutility)?
While I agree with what is proposed here in principle, the larger challenge comes from understanding the mobility of our society in a geographic sense. Defining the local/regional scope in a way that allows for actual quantification of the various harm metrics assumes a clear segregation of population. What this approach misses is the interaction and flow between segmented cohorts of quantification. To this end, the simple 2D matrix model needs to be supplemented with a network model that captures individual cohort scopes as ‘nodes’ in the network and the relationships between these cohorts as ‘edges’ to represent characteristics of the inter-cohort exchange. A simple example here – consider teachers and schools. How does having a broad range of teachers from areas different from that of the school where they teach affect calculation and estimation of risks and harms for the school community or the home community of the teacher? With an understanding of the interconnected network of cohorts we can attempt to solve the higher dimensional optimization problem across all cohorts/scopes. This concept of a index of the minimal risk surface – as opposed to simply an index of one scope or cohort – would be a more comprehensive way to address cohort iniquity and differentials across the societal space.
Pingback: No, COVID statistics don’t look bad because the US does too much testing or because hospitals are attributing too many deaths to COVID – Reward Health
Pingback: CDC’s new $200M Center for Forecasting and Outbreak Analytics mistakenly frames modeling efforts as “forecasting.” It should be all about policy decision support. – Reward Health
Pingback: A helpful analogy: Driving an 18-wheeler on a steep grade road from the top of Covid Susceptibility Mountain down to the Valley of Herd Immunity. – Reward Health